Demystifying digestive symptoms, prebiotics and probiotics
April 12, 2024 7 min read
Digestive problems are rampant in the United States and elsewhere for many reasons. One of the most common reasons is due to an imbalance of gut flora (good bacteria).
How do we feed these little critters? Should you simply swallow probiotic pills every day and call it a day?
What about prebiotics – the indigestible food that your gut bacteria need to thrive and grow? Could taking prebiotics be bad for some people?
The answer to that is "yes"! And what about FODMAPs?
The term FODMAPs is an acronym, deriving from "Fermentable Oligo-, Di-, Monosaccharides And Polyols." These carbohydrates are commonly found in the modern western diet. Evidence suggests that reducing FODMAPs in your diet can alleviate irritable bowel syndrome and other functional gastrointestinal disorders (FGID).
If you have a chronic digestive problem, you may be feeling overwhelmed by what's out there about your gut health. The first place to start is by tracking what you eat for a week, and closely monitoring associated symptoms. Those headaches and skin breakouts may be directly linked to what’s breeding in your gut!
The following excerpt from Dr. Lani’s No-Nonsense Bone Health Guide will help you untangle the symptoms of gut health imbalance:
Bacteria in the Gut
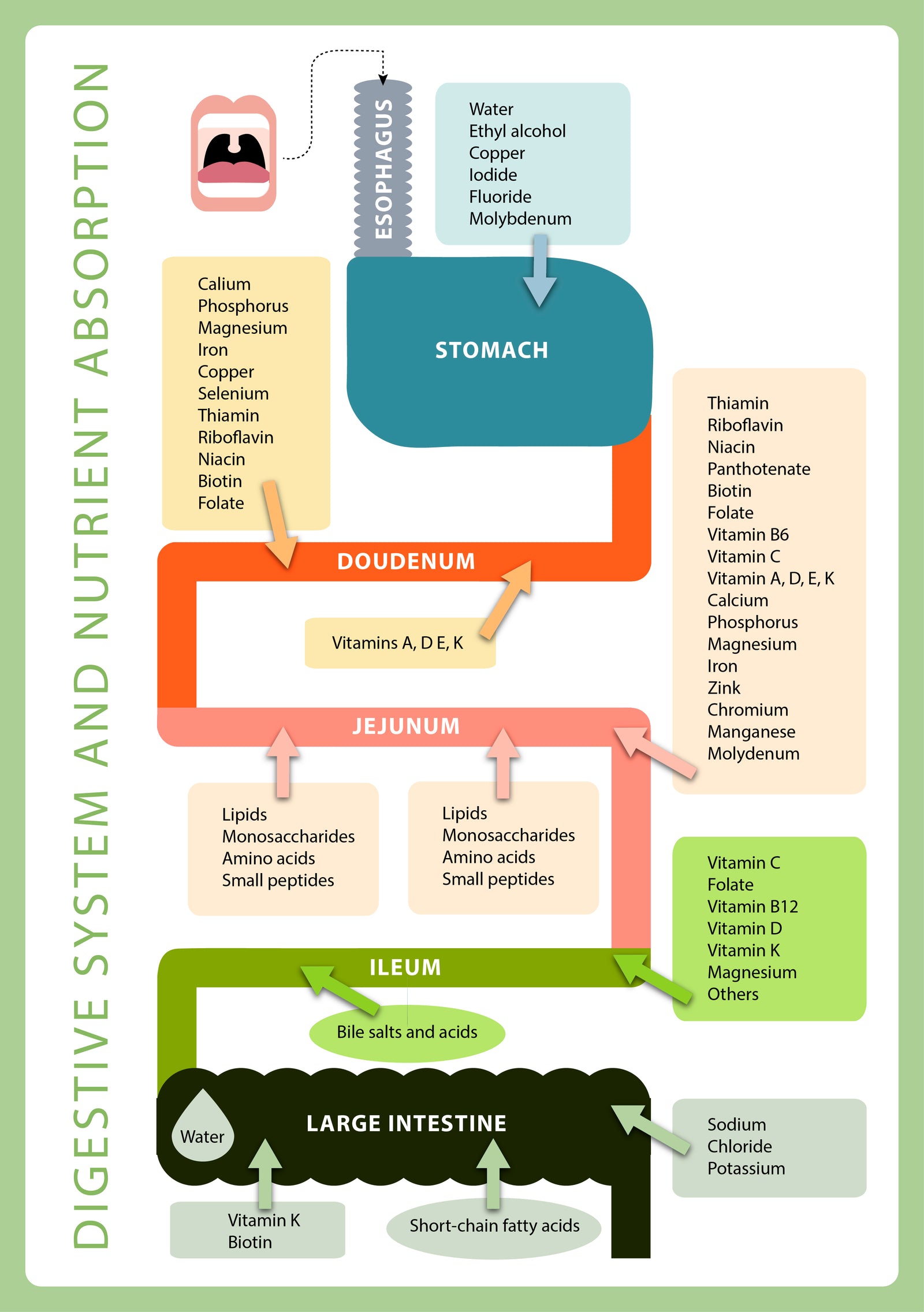
Both the small and large intestines are teeming with healthy bacteria whose main role is to assist in the breakdown of undigested carbohydrates.
It is essential to keep the “good” bacteria that aid digestion in balance if the digestive tract is to remain healthy and nutrients are to be absorbed properly. For example, the absorption of B-12 is aided by healthy gut flora.
Many older adults are deficient in this vitamin, and studies have shown that B-12 deficiency is one of the risk factors associated with bone loss. In my webinars on digestive health, we discuss how to keep these gut critters in balance to make sure you harbor enough of the good guys.
How Do You Know If You Have a Digestive Problem?
How do you know if your digestive system is not working as it should? The symptoms to watch for—for example, flatulence, diarrhea, constipation, and heartburn—can occur occasionally in people with perfectly healthy digestion. But they should be infrequent issues, not constant burdens.
In fact, it is extremely common for women to experience loose stools or constipation around their menstrual cycle or during pregnancy as a result of hormonal changes. As is the case with most bodily systems, the occasional irregularity in the GI system doesn’t indicate a chronic issue, just as an occasional headache doesn’t signify a brain tumor.
But symptoms such as those listed below that occur daily or even weekly are signs that something is impacting the digestive tract—something that, over time, could lead to problems throughout the entire body.
Some of the most common signs and symptoms of gastrointestinal problems include:
- excessive gas, bloating, burping, or flatulence
- heartburn or GERD
- food sensitivities
- stomach cramps or nausea
- abnormal stools
- abnormal bowel habits (e.g., constipation, diarrhea, taking a long time to void the bowels)
- itching or burning of the rectum
Furthermore, other chronic symptoms that most people don’t think of as GI-related can also indicate a problem in the GI system, for example:
- skin irritations, rashes, eczema
- headaches
- fatigue
- anxiety or depression
- joint or muscle pain
- unexplained weight gain or weight loss
Please note that I am not saying these additional symptoms are necessarily GI-related—but they might be, depending on their cause. Weight gain, for example, can be caused by insufficient intake or absorption of the B vitamins, iron, magnesium, and other nutrients needed to help the body burn calories.
Bottom line: If your body is not getting the nutrients it needs, you may experience a wide range of problems—and not just those we typically think of as tied to the digestive tract.
Where to Look First: Taking the Taboo Out of Poo
The head bone’s connected to the neck bone, the neck bone’s connected to the back bone—and they’re all connected to the gut. In my practice, one of the first things I assess when I see a client who presents with bone loss is their digestive health.
Before their initial visit, along with completing a nine-page questionnaire, my new clients are tasked with keeping a seven-day diet and symptom journal, which gives me an idea of their food choices, nutrient intake, and digestive health.
During a client's first appointment, I candidly discuss their GI symptoms, and some of the most important questions I ask concern their bowel movements. Granted, the topic is not one most people want to discuss, but knowing about someone’s stools gives me a lot of information about how their digestive tract may or may not be working.
(**Please note: as of 2024, Dr. Lani is not taking new patients**)
Everyone has abnormal bowel movements from time to time due to illness, or as a reaction to a food substance (or something else) that has been ingested.
However, if you have abnormal bowel movements on a regular basis, it may be a significant sign that something is not right with your body. Color, odor, texture, and consistency are all aspects of a person’s stool that can provide clues about whether or not the GI tract is working as it should.
Following is a brief overview of what to look for when it comes to bowel movements.
Stool Color
Color tells us a lot about when stools are abnormal. The color of a healthy stool is brownish, but a white or very pale-colored stool, for example, can indicate that the gallbladder is not releasing enough bile (bile has a greenish color, which darkens the stool).
Red streaks, red spots, or other reddish areas in the stool may indicate the presence of blood from either the descending colon or the rectum. Blood that has traveled from the stomach or intestines may produce dark or blackish stools.
The most common cause of red blood in stools is a bleeding hemorrhoid, but blood in the stool can also be an early warning sign of cancer, so don’t ignore it. Red beets can produce red stools (and urine), and Pepto-Bismol can cause very dark stools.
Constipation
Everyone has experienced constipation from time to time; it is one of the conditions with which my clients most often present. Some of the symptoms include abdominal pain, gas, and bloating, but constipation can also cause fatigue and even permanent damage to the colon.
Although occasional constipation is nothing to worry about, pain with bowel movements or straining on a regular basis is not normal; a bowel movement should be effortless.
Following are some of the main causes of constipation:
- dehydration
- insufficient magnesium intake
- a low-fiber diet
- diverticulosis (out-pocketing in the large intestine)
- hemorrhoids
- irritable bowel syndrome (IBS)
- excessive intake of protein and/or dairy products
- hypochlorhydria (low production of hydrochloric acid in the stomach)
- insufficient physical activity
- pelvic floor dysfunction (caused when the muscles that are used to move the bowels aren’t properly coordinated)
- certain hormonal disturbances, for example, hypothyroidism
- certain medications, for example, those that contain codeine (always read drug labels for possible side effects)
For many people, constipation can be easily fixed with dietary and lifestyle changes that include whole foods, more exercise, more water, fiber-rich foods, and enough magnesium in the diet to balance calcium. (You’ll learn how to balance these two minerals in my webinar.)
Loose Stools
Diarrhea, or loose stools, can be caused by digestive disorders, infections, or dietary intake of certain foods or food additives. Whereas everyone experiences transient episodes of loose stools from time to time, chronic diarrhea means that you may not be absorbing the nutrients you need, which in turn can lead to significant problems—for example, bone loss.
Some of the main causes of chronic diarrhea include:
- high intake of sugar alcohols, found in diet drinks and diet foods (if you’re someone who reads food labels, watch for ingredients such as xylitol, sorbitol, mannitol, lactitol, isomalt, maltitol, or hydrogenated starch hydrolysates)
- poor diet choices or overindulgence in certain foods, especially sugar and greasy junk foods such as potato chips
- candida overgrowth (candida is a yeast that lives in the intestines; see below for more information)
- certain medications, including antibiotics, antidepressants such as Zoloft and Prozac, and corticosteroids (e.g., prednisone)
- certain food intolerances (for example, lactose intolerance or celiac disease)
- pancreatic insufficiency (which leads to low output of digestive enzymes)
- gallbladder impairment (which leads to low output of the gallbladder’s digestive juices)
- irritable bowel syndrome (IBS)
- leaky gut syndrome
- autoimmune diseases of the intestines, for example, Crohn’s disease, ulcerative colitis, or celiac disease
- food poisoning
- infections
Mucus
Whitish mucus in the stool may be a sign of an intestinal disease. Small amounts of mucus in the stool are normal, but irritable bowel syndrome, celiac disease, diverticulitis, ulcerative colitis, bacterial infections, and Crohn’s disease may lead to amounts that are greater than normal.
Fatty Stool
Steatorrhea, or the presence of excessive fat in the stools, is one of the main signs of malabsorption conditions such as gluten intolerance (described in more detail later in the chapter).
Fatty stools are often oily and foul smelling; they may float or stick to the side of the bowl, making it difficult to flush them away.
The Bristol Stool Chart is another tool that can help you identify whether your stools are normal. The chart classifies human stool in terms of seven categories, using both illustrations and written descriptions to describe each stool form.
The Bristol stool types are described below, and you can also download the chart.
The Bristol Stool Types
| Type | Description | Analysis |
| 1 | Separate, hard lumps, like nuts. Hard to pass, indicating constipation. | Abnormal |
| 2 | Sausage-shaped and lumpy. Hard to pass, indicating constipation. | Abnormal |
| 3 | Sausage-shaped with cracks on the surface, leaning toward constipation. | Abnormal |
| 4 | Sausage-shaped or snake-shaped, smooth, and soft. May have a curve. Easy to pass. | Normal |
| 5 | Soft blobs with clear-cut edges. | A normal variant |
| 6 | Fluffy pieces with ragged edges, mushy, leaning toward diarrhea. | Borderline abnormal |
| 7 | Watery, no solid pieces. | Abnormal |
The Bristol stool chart is a useful tool; however, it does not include important symptoms such as color or odor, and there is some disagreement as to the normality or abnormality of some of the types. For example, some experts view type 3 as normal. In my opinion, and that of other health-care practitioners, this type is not normal but rather indicates a mild form of constipation.
Bowel movements should be effortless, and they should occur at least once a day. Some medical references state that constipation is defined by a failure to defecate within a three-day period. I strongly disagree with this assessment.
Though failure to defecate once each day may be the norm in a society that eats a typical American diet, it indicates sub optimal functioning. In fact, a diet that is high in fiber usually produces more than one healthy bowel movement each day.
Conclusion
Adding fiber to the diet can be tricky for some people. Come learn about healthy fibers, both soluble and insoluble as well as probiotics, prebiotics, and FODMAPs in Dr. Lani’s upcoming masterclass on April 17t, 2024. You can join the masterclasshere.
Subscribe
Sign up to get the latest on sales, new releases and more …

